Rural Health Transformation Program (RHTP)
A Request for Information (RFI) has been conducted, closing September 24, 2025, to solicit input from stakeholders to inform the Louisiana Department of Health’s (the Department) application to the Centers for Medicare & Medicaid Services (CMS) Rural Health Transformation (RHT) Program. The Department’s vision for this program is to provide transformative changes with long-lasting health impacts for rural Louisianans.
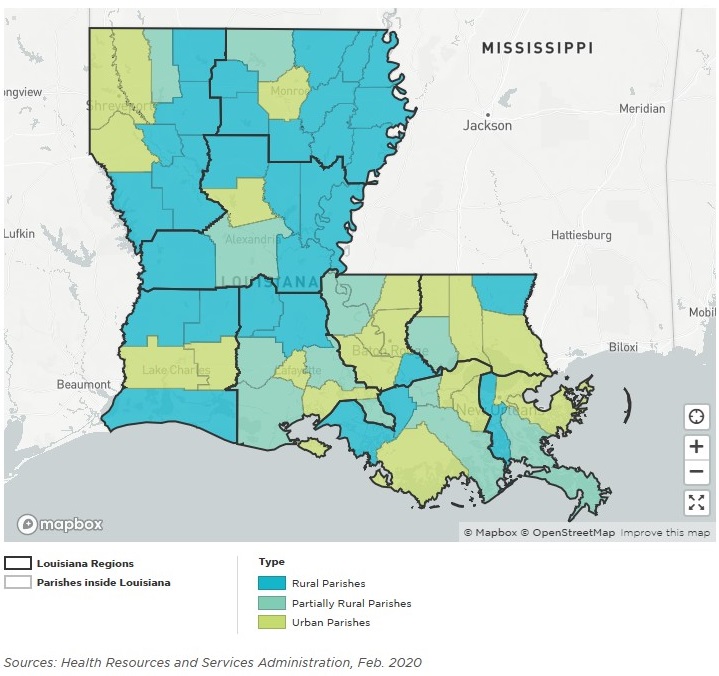
Louisiana's Rural Landscape
44 of Louisiana’s 64 parishes are designated as fully or partially rural, and approximately 29.1% of Louisiana’s population lives in rural areas.
Primary Care
73% of Louisiana residents live in a Primary Care Health Professional Shortage Area.
Mental Health
93% of Louisiana residents live in a Mental Health Professional Shortage Area.
Dental Health
86% of Louisiana residents live in a Dental Health Professional Shortage Area.
11% of adults in rural Louisiana have heart disease.
32% higher than urban prevalence of 8%.
20% of adults in rural Louisiana have diabetes.
42% higher than urban prevalence of 14%.
43% of adults in rural Louisiana are obese.
21% higher than urban prevalence of 38%.
39% of adults in rural Louisiana use tobacco.
12% higher than urban prevalence of 27%.
56% of new HIV cases are from outside New Orleans and Baton Rouge.
RHTP Overview
- Section 71401 of the Reconciliation Bill allocated transformative funding to rural health systems – strategic readiness is critical.
- $50 billion earmarked over 5 years for rural health infrastructure, workforce, and access.
- Prioritizes underserved areas with high morbidity and provider shortages.
- Must submit transformation plans by a tight timeframe, as determined by CMS.
Funding
- $50 billion from Federal Fiscal Years 2026 through 2030; $10 billion each fiscal year.
- ○50% of funding divided equally among all states with approved application.
- ○50% distributed in amount determined by CMS administrator
- % of state population located in rural census tract of metropolitan statistical area.
- Proportion of rural health facilities in state relative to number of rural health facilities nationwide.
- Situation of hospitals in state.
- Any other factor CMS deems appropriate.
- Funds must be used by end of the fiscal year following the fiscal year in which funds were allotted.
- No more than 10% state administrative expenses.
- State match not required.
Use of Funds
- Improve prevention and chronic disease management.
- Payments to health care providers for provision of health care items or services.
- Technology-driven solutions for prevention and management of chronic diseases.
- Providing training/technical assistance for technology-enabled solutions.
- Recruiting/retaining clinical workforce.
- Technical assistance, software, and hardware for significant information technology advances.
- Right-size health care delivery systems by identifying needed preventative, ambulatory, pre-hospital, emergency, acute inpatient care, outpatient care and post-acute care service lines.
- Improve access to opioid use disorder and other substance use disorder treatment services, and mental health services.
- Value-based care arrangements and alternative payment models.
- Additional uses to promote sustainable access to high quality rural health care services.
Plan Requirements
- Improve access to hospitals, other health care providers, and health care items and services furnished to rural residents of the state.
- Improve health care outcomes of rural residents of the state.
- Prioritize use of new and emerging technologies that emphasize prevention and chronic disease management.
- Initiate, foster and strengthen local and regional strategic partnerships between rural hospitals and other health care providers to promote measurable quality improvement, increase financial stability, maximize economies of scale, and share best practices in care delivery.
- Enhance economic opportunity for, and the supply of, health care clinicians through enhanced recruitment and training.
- Prioritize data and technology driven solutions that help rural hospitals and other rural health care providers furnish high-quality health care services as close to patient’s home as possible.
- Outline strategies to manage long-term financial solvency and operating models of rural hospitals.
- Identify specific causes driving accelerating rate of stand-alone rural hospitals at risk of closure, conversion or service reduction.
- Certify use of funds - will not be used for intergovernmental transfers, certified public expenditures, or any other expenditure that finances the non-federal Medicaid share.
- Any other information that CMS administrator may require.
Rural Health Facilities
- Rural health clinic
- Federally qualified health center
- Community mental health center
- Opioid treatment program
- Health center receiving a grant under section 330 of the Public Health Service Act
- Certified community behavioral health clinic located in rural census tract
Hospitals meeting specific rural or hospital-type criteria defined in Title XVIII of SSA:
- Critical access hospital
- Sole community hospital
- Medicare-dependent, small rural hospital
- Low-volume hospital
- Rural emergency hospital
- Medicare subsection (d) hospital in rural area
Contact
For more info or to share your ideas, email [email protected].
 Official Louisiana State Websites use .la.gov
Official Louisiana State Websites use .la.gov  Secure .gov websites use HTTPS
Secure .gov websites use HTTPS