About Louisiana Sickle Cell Disease
What is Sickle Cell Disease?
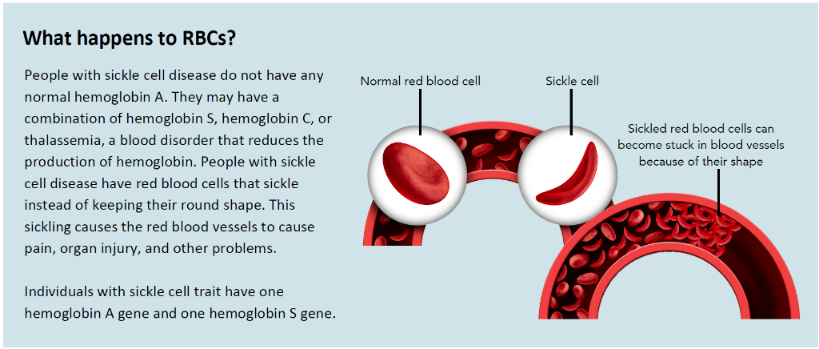
Sickle cell disease (SCD) is a group of red blood cell disorders that are inherited (passed down from parents or family members). Red blood cells contain hemoglobin, a protein that carries oxygen. Healthy red blood cells are round, and they move through small blood vessels to carry oxygen to all parts of the body.
In someone who has sickle cell disease, the hemoglobin is not normal, which causes the red blood cells to become hard and sticky and look like a C-shaped farm tool called a sickle. The sickle-shaped cells die early, which causes a constant shortage of red blood cells. The cells become stuck in small blood vessels, which limits blood flow.
Click the links below to navigate to different topics:
- Louisiana Sickle Cell Commission
- Regional Clinics & Foundations
- Sickle Cell Disease in Louisiana
- Sickle Cell Disease Registry
- Sickle Cell Disease Resources
- Tips to Live a Healthy Life with Sickle Cell Disease
- Treatment for Sickle Cell Disease
Causes of Sickle Cell Disease
Sickle cell disease is a genetic condition that is present at birth. It is inherited (passed down) when a child receives two genes – one from each parent – that tell the body to make abnormal hemoglobin. Normal hemoglobin genes are hemoglobin A. Abnormal hemoglobin genes include hemoglobin S or hemoglobin C. People with sickle cell disease either have thalassemia, a blood disorder that produces less hemoglobin, or a combination of the two abnormal hemoglobin gene types (S or C). People with sickle cell trait (someone who can pass down sickle cell genes, but does not have the disease) have one normal hemoglobin gene (A) and one abnormal hemoglobin gene (S or C).
Diagnosis of Sickle Cell Disease
A simple blood test can detect the type of hemoglobin that causes sickle cell disease. In the U.S., this blood test is part of routine newborn screening tests at hospitals. Adults and older children can request a physical exam and blood testing from a healthcare professional to determine if the sickle cell gene is present or detect other diseases associated with the sickle cell gene.
Early diagnosis and treatment are important because of the increased risk of infection and other health problems. A healthcare professional may recommend additional testing to check for possible complications of sickle cell disease.
Complications of Sickle Cell Disease
Sickle cell disease can affect any major organ and lead to many complications. Each person with the disease can experience different symptoms and complications ranging from mild to severe. Symptoms and health effects usually begin around five months of age.
Common health complications with sickle cell disease include:
-
Pain: Sickled cells traveling through small blood vessels can get stuck and block blood flow throughout the body, causing pain. A vaso-occlusive episode (pain crisis) can start suddenly, be mild to severe, and can last for any length of time. People living with sickle cell disease can experience acute pain (comes suddenly and lasts for a short time), chronic pain (daily, ongoing pain lasting more than six months), or both.
-
Lung Problems: Acute chest syndrome, pulmonary hypertension, and sleep-disordered breathing are lung-related complications caused by sickle cell disease.
-
Organ Damage: Because not enough blood is reaching organs, people with sickle cell disease are at greater risk for organ damage, including problems with the liver, spleen, and kidneys.
-
Circulation Issues: Sickled cells commonly get stuck in blood vessels, causing many complications, including blood clots, strokes, painful swelling in the hands and feet, and more.
-
Fevers and Infections: Fevers can be the first sign of an infection or other health complications due to sickle cell disease.
Treatment for Conditions Related to Sickle Cell Disease
The primary objective of managing sickle cell disease is to avoid vaso-occlusive episodes, relieve symptoms, and prevent complications. Treatment depends on the patient's symptoms, age, general health, and the severity of the condition. Early diagnosis and preventing further problems are critical in treating sickle cell disease, and treatment goals include preventing organ damage (including strokes), preventing infection, and treating symptoms.
Treatment for sickle cell disease may include:
-
Pain Medicines: These are used for sickle cell crises (vaso-occlusive episodes).
-
Drinking Plenty of Water Daily: Doing so can prevent and treat pain crises. In some cases, IV (intravenous) fluids may be needed.
-
Blood Transfusions: These may help treat anemia (low red blood cells) and prevent stroke. They are also used to dilute the sickled (or abnormal) hemoglobin with normal hemoglobin. It is done to treat chronic (ongoing) pain, acute chest syndrome, splenic sequestration, and other emergencies.
-
Red Blood Cell Exchange: This process removes some abnormal red blood cells and replaces them with healthy red blood cells from a donor. This can help improve symptoms.
-
Vaccines and Antibiotics: These are used to prevent infections.
-
Folic Acid: This B vitamin helps prevent severe anemia.
-
Hydroxyurea: Medication that helps reduce the frequency of pain crises and acute chest syndrome. It may also help decrease the need for blood transfusions.
-
Voxelotor: Medication that is approved for people aged four and older to reduce pain crises and improve anemia caused by red blood cell destruction.
-
Crizanlizumab: Medication that is approved for people age 16 and older to reduce pain crises
-
L-glutamine: This medicine is approved for people aged five and older to reduce pain crises.
-
Regular Eye Exams: These are done to screen for an eye condition called retinopathy.
-
Bone Marrow Transplant: A transplant can cure some people with sickle cell disease. The decision to have a transplant is based on the severity of the disease and finding a suitable donor. These decisions need to be discussed with your provider. Transplants are done only at specialized medical centers.
-
Gene Therapy: New gene therapies have been approved to treat sickle cell disease. Talk with your provider (or your child's provider) about these treatments.
Emergency Treatment: Individuals living with sickle cell disease may need emergency treatment due to the varied health complications as a result of the disease. Most commonly, people living with sickle cell disease need emergency treatment for vaso-occlusive episodes, which are pain episodes related to sickle cell disease.
La. R.S. 40:978 sets limits and conditions on the prescribing of opioids in Louisiana, including generally limiting initial opioid prescriptions to no more than a seven-day supply.[1] Such limits and conditions may impact individuals living with sickle cell disease. Emergency physicians generally have the authority to prescribe opioids, but they may choose not to if they aren’t aware of a patient’s medical history. Individuals living with sickle cell disease need to inform their primary care provider of any visits to the emergency room in order to create a care plan to manage future vaso-occlusive episodes.
1The guidance and information provided herein are believed to be accurate and complete, but should not be utilized as a substitute for consulting the relevant statutes and rules, which control in the event of any discrepancy. The information provided herein does not constitute legal advice, which LDH is prohibited from providing to those outside the department. You should seek private legal counsel if you need legal advice regarding the issues addressed herein.
Living with Sickle Cell Disease
People with sickle cell disease can live full lives and enjoy most of the activities that people without sickle cell disease do. The following tips will help people with sickle cell disease stay as healthy as possible.
-
Find good medical care: Sickle cell disease is a complex disease. Good quality medical care from doctors and nurses who know a lot about the disease can help prevent some serious problems. Often, the best choice is a hematologist (a doctor who specializes in blood diseases) working with a team of specialists.
-
Get regular checkups: Regular health checkups with a primary care doctor can help prevent some serious problems.
-
Prevent infections: Common illnesses, like the flu, can quickly become dangerous for a child with sickle cell disease. The best defense is to take simple steps to help prevent infections.
-
Learn healthy habits: Children can, and should, participate in physical activity to help stay healthy. However, it is important that they do not overdo it, rest when tired, and drink plenty of water.
-
Get support: Find a patient support group or community-based organization that can provide information, assistance, and support. For more information about sickle cell disease, including diagnosis, complications, and treatment, click here.
-
Look for clinical studies: New clinical research studies are happening all the time to find better treatments and, hopefully, a cure for sickle cell disease. People who participate in these studies might have access to new medicines and treatment options. Patients can:
-
Ask their physicians about clinical trials.
-
Go to clinicaltrials.gov and sicklecelldisease.org
-
Sickle Cell Disease in Louisiana
There was an average of 70 infants born in Louisiana with sickle cell disease from 2021 to 2024. Louisiana Medicaid provides health care coverage to approximately 3,000 individuals living with the condition annually. The number of individuals living with sickle cell disease in Louisiana is currently unknown; however, the Louisiana Department of Health has made significant progress in developing the state’s first sickle cell disease registry.
Louisiana Sickle Cell Disease Registry
The Louisiana Sickle Cell Disease Registry was established by Act 647 of the 2022 Regular Session of the Louisiana Legislature. As specified in the authorizing statute, the Registry functions as a single repository of public health data related to sickle cell disease among people in Louisiana. Consistent with other public health monitoring systems that collect information about people with certain health conditions, the Registry aims to quantify and characterize sickle cell disease in the state; assess trends in diagnosis, treatment, and access to care; and inform public health decision-making, policy, and other actions to support the health of individuals living with sickle cell disease in the state.
Click here to learn more about the Louisiana Sickle Cell Disease Registry.
Data Sharing Agreements
In Act 748 of 2024, the Louisiana Legislature mandated LDH to “facilitate an agreement between sickle cell clinics as provided for in R.S. 40:1125.31 et seq, and an association that is part of the Louisiana Sickle Cell Commission that provides information and assistance to patients diagnosed with sickle cell disease. The agreement shall allow for the transfer of sufficient contact information from the sickle cell clinics to allow an association to contact the patient.”
In order to improve outcomes for people living with sickle cell disease, increased awareness of and access to community resources is needed. The Louisiana Department of Health can assist in facilitating data-sharing agreements between health care providers and regional sickle cell foundations by offering resources to support this process. These agreements allow for patient or family contact information to be shared with patient consent.
Health care providers may establish data-sharing agreements with regional sickle cell foundations across Louisiana to help connect patients to education, resources, and support services. The Louisiana Department of Health developed a sample data-sharing agreement template that you can adapt.
[DATA SHARING AGREEMENT TEMPLATE]
Sickle Cell Disease Program
The Louisiana Department of Health, Office of Public Health, Bureau of Family Health Genetic Diseases Program works with sickle cell clinics across Louisiana to ensure individuals living with sickle cell disease have access to care throughout the state. The program directly oversees the Monroe Sickle Cell Center in the Ouachita Parish Health Unit and the Alexandria Sickle Cell Clinic in the Rapides Parish Health Unit. These clinics provide access to hematologists and other specialist providers for individuals living with sickle cell disease in parts of the state that otherwise might not have local access. The program also contracts with sickle cell clinics in New Orleans, Lake Charles, Shreveport, Alexandria, and Monroe.
In addition to the Bureau of Family Health’s work with clinical systems, the Bureau also provides support to sickle cell foundations statewide and provides funding for five sickle cell foundations, located in Baton Rouge, Lake Charles, Alexandria, Shreveport, and Monroe. Sickle cell foundations are community-based organizations that have programs that link individuals and families affected by sickle cell disease with medical and non-medical resources needed to manage this complex disease. The foundations also help to ensure all infants diagnosed with sickle cell disease through the Newborn Screening Program are linked to appropriate care upon diagnosis. Click here to see the full list of sickle cell foundations and clinics around the state.
This program also oversees the Louisiana Sickle Cell Commission, which is mandated by Act 117 (Senate Bill 57) of the 2013 Regular Session of the Louisiana State Legislature. Click here to find information on the Louisiana Sickle Cell Commission, including meeting dates, agendas, and minutes. For the most recent Commission report, including information on current appointments, click here.
Sickle Cell Disease Resources
Resources for Healthcare Providers
The Louisiana Standard for Care of Patients with Sickle Cell Disease serves as a best practices guide for treating patients with sickle cell disease. It was developed by Renee Gardner, MD, a pediatric hematologist with Louisiana State University Health Sciences Center in New Orleans and the Louisiana Sickle Cell Commission. The goal of the toolkit is to increase and improve access to reduce acute pain and improve chronic pain management. The toolkit is distributed to pediatricians, family practitioners, and other primary care providers to follow as best practices for treating patients with sickle cell disease.
Individuals living with sickle cell disease may frequently visit the emergency department to seek care and manage vaso-occlusive (severe pain) episodes and other symptoms related to the disease. Many people with sickle cell disease report unique barriers and challenges, such as long wait times and a lack of provider knowledge related to sickle cell disease, when seeking treatment in emergency department settings. Providers in emergency departments can use resources found in the Sickle Cell Disease Pain Management Toolkit to improve care for people with sickle cell disease when they are in the emergency department. This toolkit provides information about sickle cell disease and recommendations for emergency department providers.
Resources for Patients and Families
The Office of Public Health can provide resources and information for people diagnosed with sickle cell on how to receive assistance and care through the sickle cell foundations and clinics around the state. Click the links below to learn more about sickle cell foundations across Louisiana.
-
Louisiana Sickle Cell Foundations:
Additional Resources
The U.S. Centers for Disease Control and Prevention has compiled stories from people directly affected by sickle cell disease, highlighting the impact that identification, treatment, and resources can have on real people. Read their stories here.
-
Family Resource Center: The Family Resource Center helps identify and connect families to resources and services in their community and across the state based on their child’s specific needs. They can also connect families to resources related to insurance, finances, education, food security, and more.
-
Addressing Sickle Cell Disease: A Strategic Plan and Blueprint: This strategic plan is from the National Academies, which examines the epidemiology, health outcomes, genetic implications, and societal factors associated with sickle cell disease and sickle cell trait.
-
CMS Sickle Cell Disease Provider Toolkit: This toolkit is from the U.S. Department of Health & Human Services (HHS) Centers for Medicare & Medicaid Services (CMS). This toolkit consists of six sections that will equip healthcare providers in delivering quality care to individuals living with sickle cell disease. Topics included are: 1) screening and diagnosis; 2) treatments; 3) comprehensive care; 4) CMS programs and resources; 5) resources to support multi-disciplinary care across settings; and 6) resources for individuals living with sickle cell disease.
-
Sickle Cell Disease Toolkit for Schools: Students who live with sickle cell disease are more at risk for emotional and social complications. Because of these symptoms and complications, students may be more likely to miss school or perform poorly in school. Children living with sickle cell disease are also at higher risk for learning difficulties. However, there are many small things that the school community can do to help a student living with sickle cell be more successful in school. School communities can make a difference in the lives of students with sickle cell disease by understanding key facts about the disease, symptoms, and providing special accommodations.
 Official Louisiana State Websites use .la.gov
Official Louisiana State Websites use .la.gov  Secure .gov websites use HTTPS
Secure .gov websites use HTTPS